International Journal of Scientific & Engineering Research, Volume 4, Issue 9, September-2013 2283
ISSN 2229-5518
“URETERIC CATHETERIZATIONS IN UROLOGICAL PROCEDURES, A MODIFIED METHODOLGY.”
Dr.Anil K.Sahni MS, FICS, Advanced DHA, Surgeon, Medical Teacher
“ABSTRACT”-INTRODUCTION : Ureteric Catheterization Is Extensively Used In Various Urological Procedures:(I)Open Classical Surgical Procedures:Open Stone Surgery(OSS) Etc.(II)PCNL, Per-Cutaneous Nephrostomy(III) ESWL: In Large Stone Size, High Density Cases, To Avoid Stein-A- Strasse (IV) Lap. Uretero-Lithotomy, Endoscopy:Retro-Grade PyeloGraphy(RGP), Uretero-RenoScopy (+-) Lithoclast Etc.(V) Drainage Procedures- External/ Internal, Ureteric Sampling, Inf. Localization.
AIMS/OBJECTIVES : Double-J-Stent/J-J Stent(DJS) Are Commonly Available Appliances In Cl. Practice, For Ureteric Patency Achievement During
Different Surgical Proedures. Sometimes Pig Tail Catheters Are Employed. The Present Study Deals With The SucessFul Use Of Commonly Available Infant Feeding Tubes(IFTs)No.5/6 Usually & Sometimes No.7/8,To Achieve Reno-Vesical(R-V)Patency During Various Surgical Procedures Involving Pyelotomy,Nehrotomy,Calycotomy Repairs, Ureteric Anastomosis Etc.
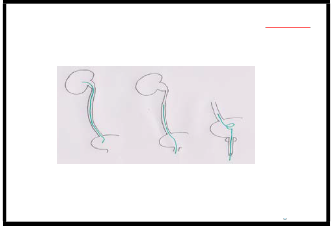
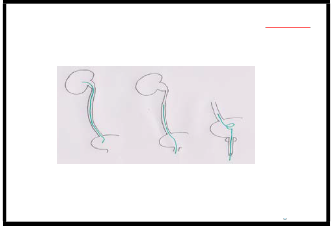
METHODS :SuccessFul Use Of Infant Feeding Tubes, As Ureteric Patency Catheterization, Done In Hundreds Of Patients Undergoing Pyelo-Plasty, Pyelo- Lithotomy, Nephro-Lithotomy,Calyco-Lithotomy, Uretero-Lithotomy,Lap.Uretero-Lithotomy , Renal /Ureteric Tumor Surgeries, Ureteric Strictures EndToEnd Anatomosis,Ureteric Trauma Surgeries Etc. After Stone Extraction,Tumor/Stricture Excision,Recostructive Repairs,Approriate Size Infant Feeding Tube Obliquely Cut At Both The Ends, Is Negotiated From Pyelotomy/ Ureterotomy W ound, First DownW ards To U.B,Confirmed By Coming Out Of Urine On Suction With A Syringe,& Then The Upper Oblique End W as Gradually Manipulated To Renal Pelvis Or Desired Pelvicalyceal Position.
For Maximal RV Drainge.Pyelotomy & Ureterotomy W ounds W ere Meticulously Secured W ith Discrete 3-0 Sutures,Avoiding Subsequent Narrowing.Surgical
Wound Closed In Layers, With Peri-Renal/Peri-Uretric Drain,Had Very Small Amount Drainage, Due To Patent Reno- Vesical Tract,Allowing Proper Healing
Of Pyelotomy/Ureterotomy.The Drainge Becoming Absolutely Dry,In 2-3 Days Time, W ere Removed.
RESULTS : The Comparative Evaluation Assessments For Use Of DJS / Infant Feeding Tubes, To Achieve Ureteric Patency As Described In Above
Mentioned Procedures,Has Been Studied As: -Comparatively Very Low Cost, Yet Easy Availability Of Needed Different Calibres Of IFTs,In Sterile Packs.
-Simplicity Of Insertion, Placement, With Ensured Reno-Vesical Patency,Avoiding Hazards Of Comparatively Much Costlier DJS Insertion & Secured
Placement To UB Below & Kidney Above, Retaining Proper Curls & Positioning,Needing Not Readily Available Guide-W ires Etc.
-The Most Important Advantage Of IFTs Use, Being Their Spontaneous Passage W ith Urine In About A W eek Time,In About More Then 90-95% Cases. Aware Patients Are Advised To Pull Out Pouting TubeThroughUrethral Orifice WithOut Getting Panicky.
Spontaneous Passage Ratio Being Higher In Female Patients.In Some Females Patients Retained IFTs In U.B, Not Able To Pass Per Urethra,Had Been
Removed Safely, With Simple Haemostat,Under Cautious Radiological Screening.
-Spontaneous Passge Of IFTs Thus Minimize Procedural Needs For CystoScopic Removal Of DJS,Necessary In All Cases Of DJS Insertion,With OverAll
Comparative SuccessFul Result Out Comes, In Regards To R-V Patency Aspect.
CONCLUSION : The AlterNative Use Of IFTs Instead Of DJS, Can Be Advocated, As An Accomplished Modified Methodology, As In Described Circumstances,With The Advantages Of Comparative Result Out Comes,Very Low Costs, Avoiding Hazards Of Availability, Difficulty During Insertion & PlaceMent Needing Added Appliances For Positioning & Complete Cystoscopy System W ithExpertise, At The Time Of Removal.
HowEver For Extensive Urology, Gynacecological, Pelvic Surgeries, Surgical Oncolgy Procedures,The Available Use Of Needed DJS/PigTail
Catheters, Is Recommended.
KEY WORDS:1.Ureteric Catheterizations 2.Ureteric Stents 3.Stent Symptoms 4.Ureteric Calibration & Patency Maintainece
5. Infant Feeding Tubes(IFTs) Use Comparative Evaluation.
1.INTRODUCTION
‘Ureteric Catheterization’ Is Extensively Used ‘Manovure’ In Various Urological Procedures,With An AimTo Achieve-
1. Benign Or Malignant Obstruction Relieve
2. PeriOperative Placement For Identification Of Ureters eg
Pelvic Surgeries,AlignMent Of Drainage System
Maintainence Of Luminal Calibre & After Ureteral
Interventions(URS) To Avoid Spasm WithHealing Felicitation.3. As An Adjunct To Stone Surgery- For ESWL, Intra-Luminal Lithotripsy, Ureteral Instrumentation &
For Stone Visualization.4. For Urinary Leak ManageMent – Leak Due To Trauma Or Surgery, Leak From Ureteral
Fistula.The Various Different Applicabilities Include- (A.)OPEN CLASSICAL SURGICAL PROCEDURES:
• OPEN STONE SURGERY(OSS): Pyelo- Lithotomy,Nephro-Lithotomy,Uretero-Lithotomy
• PUJ Obstructions,Tumor Surgeries Resections-------
--------------------------------------------------------------------
Dr. Anil K. Sahni
A-1 / F-1 Block-A Dilshad Garden
Delhi –
110095.India.
Mobile.; 09873083100
E-Mail;dranil_sahni@yahoo.co.in dranil-sahni@hotmail.com
• Ureteric Anastomosis Procedures;Strictures
• Tumors,Ureteric Line Accomplishments
• ?Retro-Peritoneal Fibrosis,
• Ureteric Kinks D/T Visceroptosis Etc
• VUJ Stones;Ureteric Orifice Ureterotomy
• Trauma ?Iatrogenic During Uterine Surgeries Etc.
(B.)PCNL, PER-CUTANEOUS NEPHROSTOMY(PCN)
(C.) ESWL:In Large Stone Size, High Density Cases,To
Avoid ‘Stein-A-Strasse’(Street Of Stones)
[15,16,17,18,19,20]
(D.) LAP. URETERO-LITHOTOMY,ENDOSCOPIES:
Retro-Grade PyeloGraphy(RGP),
Uretero-RenoScopy(+-) Lithoclast Etc.
(E) FOR DRAINAGE PROCEDURE: Minimal/Delayed/
Early Non-Functioning Kidneys Cases:?D/T Obstructive Uropathy, As Revealed By Renal Scans;
DTPA (+-) Forced Diuresis,
DMSA Renal Perfusion Studies Etc.
[6,7,8,9,10,11,12,13,14,21,22]
Localization OF Site Of Infection?Bacteriuria
IJSER © 2013 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 4, Issue 9, September-2013 2284
ISSN 2229-5518
DIFFERENTIALURETERALCATHETERIZATIONTEST- Also K/A Differential Renal Function Test /Split Renal Function Test, Is Performed For Determination Of Various
Functional Parameters Of One Kidney As Compared With
The Contralateral Kidney. Ureteral Catheterizations Is
Done By Cystoscopy In B/L Ureters Or
Renal Pelvis.The Simultaneous Measurements Are Made Of Urine Flow Rate,Insulin, Or PAH (If Infused), Endogenous Creatinine, Or Various Urinary Solutes From B/L Urinary Systems.
2. AIMS/OBJECTIVES
Double-J-Stent/J-J Stent(DJS) Are Commonly Available
Appliances In Clinical Practice.HowEver,
For Ureteric Patency Achievement During Different
Surgical Proedures,Sometimes ‘Pig Tail Catheters’
& Other AvailAbles Are Employed.
The Present Study Deals With The SucessFul Use Of
Commonly Available ‘Infant Feeding Tubes’ (IFT) No. 5/6
Usually & Sometimes No.7/8,TO Achieve Reno-
Vesical(R-V)Patency , During Various Surgical Procedures
Involving Pyelotomy, Nehrotomy, Calycotomy, Repairs, Ureteric Anastomosis Etc.
3. DISCUSSION
One Of The Most Common Devices Used By Urologists
,‘Ureteral Stent’ Sometimes Known As
‘Ureteric Stent’ (A Thin Tube Inserted Into The Ureter, To
Prevent Or Treat Obstruction Of The Urine
Flow From The Kidney & To Ensure The Patency Of
A Ureter.) Represent The Most Mature Application Of An Indwelling Endoluminal Splint,First Described By Zimskind Et Al In 1967, With The Intent Of Implantation For The Treatment Of Ureteral Obstruction Or Fistula. [1.2.3.4.5]

For The Purpose Of ‘Ureteric Catheterizations’ i.e To Achieve Urinary Drainage From Kidney To Urinary Bladder Or To An External Collecting System,Thin Flexible Tubes ,Depending Upon Patients’ Anatomy & Indication For Use, Different Sizes,Shapes & Constituting Material Of ‘Ureteral/Ureteric Stents’ Are Employed. Usually Variations Of Size, ‘Stents’ Length’ 5-12 Inches(12-30 Cms)
& Diametre 0.06-0.2 Inches(1.5-6 Mms) Are Available. One
Or Both Ends Of The Stents Are Curled To Retain Them
In Position, Named As JJ Stent / Double J
Stent(DJS) Or Pig-Tail Stent. SomeTimes,One End Of
Stent Has An Attached Thread, That Extends Through U.B, Urethra To OutSide Ext. Urinary Orifice, Assisting At The Time Of ‘Stent Removal’. The Constituting Stent Material Needs To Be Flexible, Durable, Non-Reactive & Radio- Opaque. [23,24]
‘STENT’ INSERTION:After Proper Diagnosis(USG,CT/CECT,PyeloGraphy:IVU, Cystoscopy;RGP Etc.)With Completely Explained Procedural Details & Written Consent, Needed Part Preparation & AntiBiotic Coverage, Under Sedation/StandBy Anaesthesia/Anathesthetic Lubrication
Jelly/Local/Regional S.A/G.A, Compliant Patient In Lithotomy Position, Cysto-UrethroScopy Is Performed, With Available Or Fibre-Optic Flexible CystoScope,With Noted Comment Upon Ext.Urethral Orifice, Different Parts Of Urethra, Veru-Montanum, Prostatic Urethra, Prostatic Lobes ?EnlargeMent, Urinary Bladder Mucosal Status,
“URETERIC CATHETERIZATIONS IN UROLOGICAL PROCEDURES . . .”
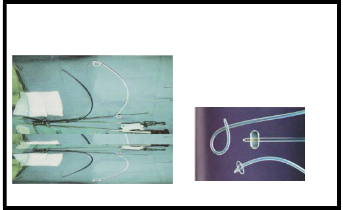
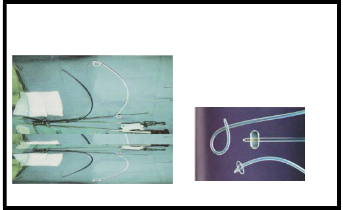
1. Double-J-Stent With Teether 2. Pig Tail & Other Catheters
Photograph 1
Trabeculations, Sacculations,Diverticulae,Other Obstructive
Uropathy Changes, Presence Of Stone, Tumour Etc.
‘BladderTrigone’ With Both Ureteric Orifices &
Intrervening InterUretric Bar Identificatied,Guide Wire Is
Negotiated Through Ureteric Orifice,Ureter To Renal
Pelvis, DJS Mounted On Guide Wire, Pushed Above By
‘Introducer’,Upper End(Curl) Is Placed In Desired Renal
Pelvi-Calyceal System & Lower End(Curl) In Urinary
Bladder. Under Available C-Arm Screening, Guided
Confirmation Plays, An Important Role. GuideWire & Cystoscopic System Is CareFully Removed. AFTERCARE;IncludesImmediate Post- OperativeCare(?Anaesthesia),
Needed Medications(Antibiotics,Analgesics Etc.),
Control X-Ray KUB For Proper Positioning With Periodic
CheckUps & Needed Management. ALTERNATIVES; In Circumstances Of Complete Ureteral Obstruction (DueTo Stone, Stricture,
Severe Spasmodic Ureteritis,Malignancy & Other Luminal
/ Intra/ Extra-Luminal Causes),
Per-Cutaneous Nephrostomy(PCN) Is PerFormed.Under
USG Guidance, Negotiated Guide Wire At The Involved Pelvi-Calyceal System Region, After Gradual Calibration Of Tract, Usually Pig-Tail Catheter Is Advanced Into Kidney & Then To Ureter & U.B, OtherWise,The Outer End Of Stent Is Connected To External Drainge System(UroBag).
STENT REMOVAL; ‘Threaded Stents’ Are Usually
Removed With Gentle, Cautious ‘Pulling Out Manovure’,
Safely In OPD. While For Stents Commonly Used
NowAdays, Complete Cysto-Urethroscopy System Is
Needed, With Anaesthesia/Sedation Provision.
SIDE EFFECTS & COMPLICATIONS; [56,57,58,59,60,61]
Main Complications -
IJSER © 2013 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 4, Issue 9, September-2013 2285
ISSN 2229-5518
Dislocation, Infection And Blockage By Encrustation. Recently Stents With Coatings Eg Heparin, Are Approved To Reduce Infection ,Encrustation & To Reduce Stent Exchanges Frequency.
Other Complications - Increased Urgency And Frequency Of Urination, Leakage Of Urine,Haematuria, Pain In The Kidney, Bladder, Or Groin, Especially After Urination.These Symptoms Are Generally Temporary And Disappear With Stent Removal.
Various Recommended Medications Are Of Significant
Help. [77,78,79,80,81,82,83,84,85,86]
Incontinence,Vesico-Ureteric Reflux,Pyuria,Fractured,
Forgotten Stent & Ureteral Erosion & Fistulization Are
Known Complications.
In ‘Threaded Stents’- Urethral Irritation Occurrence
,Especially Hypospadias Or Other Conditions
Needing SimilarCorrective Surgery,NeedsCautious Thread
Care & ‘Stent Removal’To Avoid Dislodgement.
With Properly Placed Stent In-Situ, Most Normal
Activities Are Not Effected, However Some Discomfort
During Strenuous Physical Activity May Occur.
Almost Normal Sexual Activity Can Be Achieved
InPatients With Stent, Exercising Cautious Different Sexual
Approach & Certain Barrier Contraception Use.
With ‘Threaded Stents’ Significant Hinderance Of Sex Is
Reported.
Due To Prostate Gland Movement, With Overlying Stent
, Severe Cramping, Irritation Or Discomfort
During Ejaculation/Orgasm May Occur.
IDEAL ‘URETERAL STENT’; BioCompatible,BioDurable With Better Patient Tolerance, Radio-Opaque & Or USG Visibility, Ease Of Insertion From Any Access,Migration Resistant,Optimal Flow CharacterStics, Non Refluxing, Encrustation Resistant, Ease Of Removability & Exchangebility,Verstality Yet Affordability Are The Worth Achieving, Needed Criteria.
Hydrophilic Gel Coatings Are Added To Assist Placement And Reduce Encrustation And Complicating Infection.[74,75,76]
Biodegradable Materials And Metal Stents, Are In Study
Process. [66,67,68,69,70]
Indwelling Time (Time A Stent Is In-Situ Position), Is
Usually Determined By Placement Indication Combined
With Physician Experience & Range From A Few Days For
Relief Of Ureteral Edema To Life Long Duration, For Ureteral Patency Maintenance In Malignant Diseases. Regardless Of The Stent Composition, Usual Recommendations Are For ‘Stents Exchange’
At 3- To 6-Month Intervals,While Increased Prevalence Of
Complications With Longer Indwelling Times Is Reported.
[71,72,73]
‘Case Western Reserve University’,Recorded Coding For
Kidney, Ureter And Bladder Procedures Medical Terminologies,Includes-Ureteral Stenting Codes:Pertinent Ureteral Tailoring Codes With Codes For- Cystoscopy,Pyeloplasty (Foley Y-Pyeloplasty), Plastic Operation On Ureter, Nephropexy, Nephrostomy, Pyelostomy, Or Ureteral Splinting, Simple Pyeloplasty Complicated (Congenital Kidney Abnormality, Secondary Pyeloplasty, Solitary Kidney, Calycoplasty) & Others.
3.METHODS
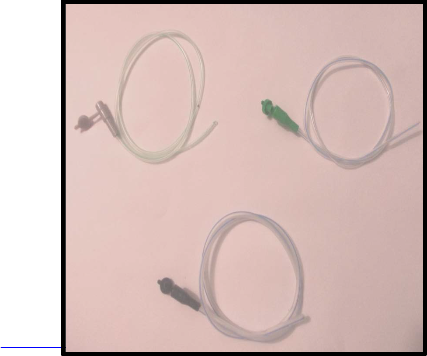
‘IFT’ INSERTION TECHNIQUE:
After Stone Extraction,Tumor/Stricture Excision, Recostructive Repair
Approriate Size Infant Feeding Tube ‘Obliquely
Cut’ At Both The Ends,Is Negotiated From
‘Pyelotomy’/ ‘Ureterotomy’ Wounds
First DownWards To U.B,Confirmed By Coming
Out Of Urine On Suction With A Syringe
Then The Upper Oblique End:Gradually
Manipulated To Renal Pelvis Or Desired
Pelvicalyceal Position
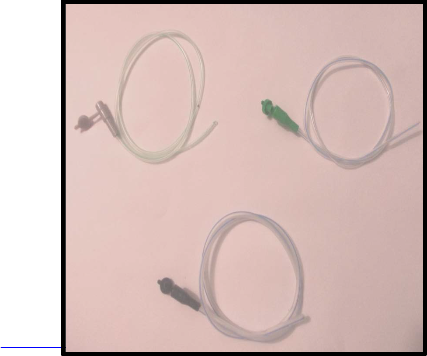
Photograph 2
IDEAL ‘URETERAL STENT’ DESIGN EVOLUTION;[23,24,25,26,27] Related Largely To Stent Material Biocompatibility & ‘Design’ To Some Extent ,
‘Stent Morbidity,Nullification/Reduction & Ideal Stent
Preparation [28,29,30,31,32,33,34]
Standardized Softness Of Silicone Material Negated By
High Coefficient Of Friction Of Silicone,
Initiated Use Of Polyethylene, But Urinary Environment
Unstablity Leading To Fracture Stents Etc.
Polyurethane Was Substituted &Continued To Be Used In
Stent Construction,Either Alone Or In Combination With
Other Materials. [35,50,51,52,53,54,55]
More Recently, Copolymers Such As C-Flex (Concept
Polymer Technologies, Clearwater, FLA),
Percuflex (Boston Scientific, Natick, Mass), And Flexima
(Boston Scientific)
Have Been Used In The Construction Of Double-J Or
Double-Pigtail Catheters. [62,63,64,65]
IJSER © 2013 http://www.ijser.or
International Journal of Scientific & Engineering Research, Volume 4, Issue 9, September-2013 2286
ISSN 2229-5518
INFANT FEEDING TUBES (IFTs) No. 5, 6 & 10
FOR MAXIMAL RENO-VESICAL DRAINGE:
• Pyelotomy & Ureterotomy Wounds, Were, Meticulously Secured With Discrete 3-0 Sutures, Avoiding Subsequent Narrowing.
• Surgical Wound Closure,In Layers, With Peri- Renal/Peri-Uretric Drain.
Post-Operative Period:Had Very Small Amount Drainage,Due To Patent ‘Reno-Uretero-Vesical Tract’ , Allowing Proper Healing Of Pyelotomy / Ureterotomy.The Drainage Becoming Absolutely Dry, In 2-3 Days Time & Removed.
The Direct Relation Of Foleys’ Catheter Removal With Ureteral Stents Retainment In-Situ & Passage Donwards Towards Urinary Bladder Outwards, Explainable By Uro-Dyanamic Fundamentals & Is Practically Monitored By’‘Peri-Nephric Drainage’Status, Once Dried, Removal Of Foleys Catheter Will Facilitate Forward Movement Of IFT, Down To Bladder & Outside Body, By Normal Urodynamics.
Wires Etc.
At Ease, Spontaneous Passage With Urine,In About A
Weeks Time,Being The Most Important Advantage Of IFTs
Use,SucessFully Recorded, In About More Then 90-95% Cases.
“URETERIC CATHETERIZATIONS IN UROLOGICAL PROCEDURES . . .”
‘RESULTS’
AT EASE, SPONTANEOUS PASSAGE WITH URINE,
In About A Weeks Time,
Being The Most Important Advantage Of IFTs Use, SucessFully Recorded, In About More Then 90-95% Cases.
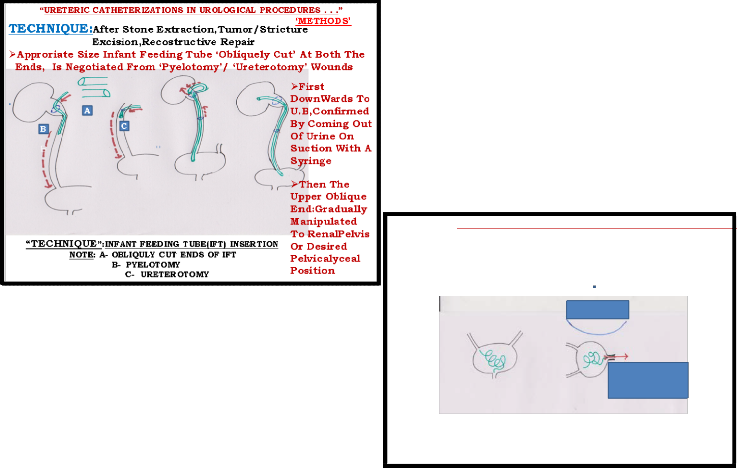
PROCESS OF SPONTANEOUS PASSAGE OF ‘IFT
SomeTimes Advised Aware Patients Are Needed To Pull Out
Pouting Tube Through Urethral Orifice WithOut Getting Panicky.
Spontaneous Passage Ratio Is Higher In Female Patients’
Figure 2
PROCESS OF SPONTANEOUS PASSAGE OF
‘IFTs’SomeTimes Advised Aware Patients Are Needed,To Pull Out Pouting Tube Through Urethral Orifice WithOutGetting Panicky.Spontaneous Passage Ratio Is More In Female Patients. Spontaneous Passge Of IFTs, Thus Minimize ProceduralNeeds For Cystoscopic Removal Of DJS, Necessary In All Cases Of DJS Insertion,With OverAll Comparative SuccessFul Result Out Comes, In Regards To R-V Patency Aspect.
OTHER SIDE-EFFECTS / COMPLICATIONS Of
‘URETHRAL STENTING:Stent Symptoms;Pain, LUTS,
Dysuria, Haematuria,Back Pain, UTI.Incorrect Placement, Migration, Stent Blockage, Forgotten Stent Etc,Can Be Cautiously Avoided By Secured Adherence, To Proper Asepsis, IFTs Procedural Technique, & Compliance Etc.
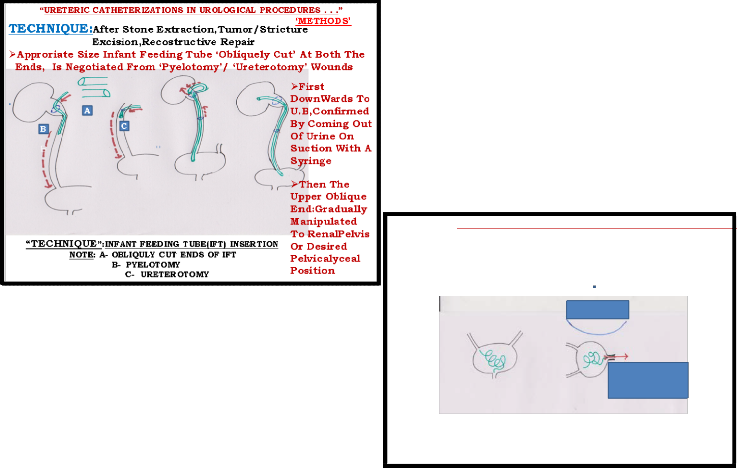
“URETERIC CATHETERIZATIONS IN UROLOGICAL PROCEDURES . . .”
‘RESULTS’
IN SOME FEMALES PATIENTS RETAINED IFTS IN U.B, NOT ABLE TO PASS PER URETHRA,
HAD BEEN REMOVED SAFELY,
WITH SIMPLE HAEMOSTAT,
UNDER CAUTIOUS RADIOLOGICAL SCREENING.
Figure 1
Radiological
Screening
4.RESULTS
The ‘Comparative Evaluation Assessments’, For Use Of
‘DJS’ & ‘Infant Feeding Tubes(IFTs)’,
To Achieve Ureteric Patency As Described In Above
Mentioned Procedures,Has Been Studied As: Comparatively Very Low Cost,Yet Easy Availability , Of Needed Different Calibres Of IFTs,
In Sterile Packs.
Simplicity Of Insertion, Placement, With Ensured
Comparative Reno-Vesical Patency Avoiding Hazards Of Comparatively Much Costlier DJS Insertion & Secured Placement To UB Below & Kidney Above, Retaining Proper Curls & Positioning, Needing Not Readily Available Guide-
With Appropriate Haemostat , Cautiously
IFT Is Pulled Out
“REMOVAL OF RETAINED ‘IFT’ IN FEMALE U.B”
Figure 3
In Some Females Patients Retained IFTs In U.B, Not Able
To Pass Per Urethra,Had Been Removed Safely,With
Simple Haemostat, Under Cautious Radiological Screening.
IJSER © 2013 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 4, Issue 9, September-2013 2287
ISSN 2229-5518
5.CONCLUSION
The Alternative Use Of IFTs Instead Of DJS, Can Be
Advocated, As An Accomplished
‘Modified Methodology’, Especially In Limited Resources Availability Circumstances.With “Secured Comparative Result Out Comes”,The Advantages Include:
• Very Low Costs,Easy Availability Of Different
Calibres, In ‘Sterile’ Packing.
• Simple, Safe Procedural Benefits, Avoiding
Hazards Of Availability, Difficulty During
Insertion & Proper PlaceMent; Positioning In-Situ.
• Avoidance Of Need For Complete ‘Cystoscopy
System’With Expertise, At The Time Of Removal.
HowEver For Extensive Urology, Gynacecological, Pelvic
Surgeries, Involving Ureteric Delineation, Reconstructive Repairs, Surgical Oncolgy Procedures,The Available Use Of Needed DJS/PigTail Catheters, Is Recommended.
6.ACKNOWLEDGEMENTS
With Special Gratitude And Thanks For,All The ‘Study Material Resources’ Consulted,Every Involved Personnel In The Surgical/Anaesthesia(Seniors & Colleagues), Para- Medical Staff Team Especially Radio-Diagnostic
Personnels, For Constant Co-Operation ThroughOut, Managing Hundreds Of Patients, In Available Resources Circumstances, SomeTimes In Very Difficult Situations, During Last More Than (2) Decades.
Dr.(Mrs)Poonam Sahni M.B.B.S,D.G.O(Gold Medalist)
For Her Accompaniment During ‘Scientific Presentation’ Of Scientific Study & Constant Co-Operation ThroughOut.
7.REFERENCES
1. Zimskind PD, Fetter TR, Wilkerson JL. Clinical use of long-term indwelling silicone rubber ureteral splints inserted cystoscopically. J Urol 1967; 97:840-844.
2. Ramsay JW, Payne SR, Gosling PT, et al. The
effects of double J stenting on unobstructed ureters. An experimental and clinical study. Br J Urol 1985; 57:630.
3. Siggers JH, Waters S, Wattis J, Cummings L. Flow dynamics in a stented ureter. Math Med Biol 2009;
26:1.
4. Venkatesh R, Landman J, Minor SD, et al. Impact
of a double-pigtail stent on ureteral peristalsis in
the porcine model: initial studies using a novel
implantable magnetic sensor. J Endourol 2005;
19:170.
5. Waterman, BJ, Jerde, T, Nakada, SY. Ureteral
physiology: implications in urological practice.
AUA Update Series 2006; Vol 25, Lesson 17.
6. Borofsky MS, Walter D, Shah O, et al. Surgical
decompression is associated with decreased
mortality in patients with sepsis and ureteral calculi. J Urol 2013; 189:946.
7. Pearle MS, Pierce HL, Miller GL, et al. Optimal method of urgent decompression of the collecting system for obstruction and infection due to ureteral calculi. J Urol 1998; 160:1260.
8. Lennon GM, Thornhill JA, Grainger R, et al.
Double pigtail ureteric stent versus percutaneous
nephrostomy: effects on stone transit and ureteric
motility. Eur Urol 1997; 31:24.
9. Ramsey S, Robertson A, Ablett MJ, et al. Evidence- based drainage of infected hydronephrosis secondary to ureteric calculi. J Endourol 2010;
24:185.
10. Sountoulides P, Pardalidis N, Sofikitis N.
Endourologic management of malignant ureteral
obstruction: indications, results, and quality-of-life issues. J Endourol 2010; 24:129.
11. Izumi K, Mizokami A, Maeda Y, et al. Current outcome of patients with ureteral stents for the management of malignant ureteral obstruction. J
Urol 2011; 185:556.
12. Docimo SG, DeWolf WC. High failure rate of indwelling ureteral stents in patients with extrinsic
obstruction: experience at 2 institutions. J Urol 1989;142:277-279.
13. Zagoria RJ. In the management of a patient with nonmalignant obstructive uropathy and known infection, isn’t it safer and more prudent to attempt retrograde placement of a ureteral stent before percutaneous nephrostomy?AJR Am J
Roentgenol 1997; 168:1616.
14. External urinary diversion: pathologic
circumstances and available technology. Macaluso
JN Jr. J Endourol. 1993 Apr;7(2):131-6. PMID
8518825Duvdevani M, Chew BH, Denstedt JD.
Minimizing symptoms in patients with ureteric
stents. Curr Opin Urol 2006; 16:77.
15. Haleblian G, Kijvikai K, de la Rosette J, Preminger
G. Ureteral stenting and urinary stone management: a systematic review. J Urol 2008;
179:424.
16. Gerber R, Nitz C, Studer UE, Danuser H. Spiral
stent versus standard stent in patients with
midsize renal stones treated with extracorporeal shock wave lithotripsy: which stent works better? A prospective randomized trial. J Urol 2004;
172:965.
17. Chen ASC, Saltzman B. Stent use with extracorporeal
shock wave lithotripsy. J Endourol 1993; 7:155-162.
18. Denstedt JD, Wollin TA, Sofer M, et al. A
prospective randomized controlled trial comparing
nonstented versus stented ureteroscopic
lithotripsy. J Urol 2001; 165:1419.
19. Chandhoke PS, Barqawi AZ, Wernecke C, Chee-
Awai RA. A randomized outcomes trial of ureteral stents for extracorporeal shock wave lithotripsy of solitary kidney or proximal ureteral stones. J Urol
2002; 167:1981.
IJSER © 2013 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 4, Issue 9, September-2013 2288
ISSN 2229-5518
20. Cass AS, Kavaney P, Levine L, et al. Extracorporeal shock wave lithotripsy for calcified ureteral stent. J Endourol 1993; 7:7-10.
21. Schlussel, RN, Retik, AB. Ectopic ureter, ureterocele, and other anomalies of the ureter. In: Campbell-Walsh Urology, 4, Wein (Ed), 2007..
22. Goldfarb RA, Neerhut GJ, Lederer E. Management of acute hydronephrosis of pregnancy by ureteral
stenting: risk of stone formation. J Urol 1989;
141:921.
23. Seymour H, Patel U. Ureteric stenting: current
status. Semin Intervent Radiol 2000; 17:351-365.
24. Denstedt JD, Reid G, Sofer M. Advances in ureteral
stent technology.World J Urol 2000; 18:237-242.
25. Chew BH, Duvdevani M, Denstedt JD. New developments in ureteral stent design, materials and coatings. Expert Rev Med Devices 2006; 3:395.
26. Davenport K, Kumar V, Collins J, et al. New ureteral stent design does not improve patient
quality of life: a randomized, controlled trial. J Urol
2011; 185:175.
27. Erturk E, Sessions A, Joseph JV. Impact of ureteral
stent diameter on symptoms and tolerability. J
Endourol 2003; 17:59.
28. Haferkamp A, Brkovic D, Wiesel M, Staehler G, Dorsam J. Role of color-coded Doppler sonography in the assessment of internal ureteral stent patency. J Endourol 1999; 13:199-203.
29. Fox CW, Jr, Vaccaro JA, Kiesling FJ, Jr, Brown SL,
Belville WD.Determination of indwelling ureteral
stent patency: comparison of standard contrast and nuclear cystography, and Lasix
renography. Urology 1994;43:442-445.
30. Ureteral stents- Materials; Endourology update:
Mardis HK, Kroeger RM: Urological Clinics of
North America, 1988, Vol. 15, No.3, 471-479.
31. Mardis HK, Kroeger RM. Ureteral stents:
materials. Urol Clin North Am1988; 15:471-479.
32. Beiko DT, Knudsen BE, Denstedt JD. Advances in
ureteral stent design. J Endourol 2003; 17:195.
33. Ureteral stents – indications, variations and complications: Saltzman B: Endourology update : Urological Clinics of North America, 1988, Vol.15, No.3, 481-491.
34. Pilcher JM, Patel U. Choosing the correct length of
ureteric stent: a formula based on the patient's height compared with direct ureteric measurement. Clin Radiol 2002; 57:59.
35. Mardis HK, Kroeger RM, Morton JJ, Donovan JM.
Comparative evaluation of materials used for
internal ureteral stents. J Endourol 1993; 7:105.
36. Tunney MM, Keane PF, Jones DS, Gorman SP.
Comparative assessment of ureteral stent
biomaterial encrustation. Biomaterials 1996;
17:1541.
37. Liu JS, Hrebinko RL. The use of 2 ipsilateral
ureteral stents for relief of ureteral obstruction from extrinsic compression. J Urol 1998; 159:179.
IJSER © 2013 http://www.ijser.org
38. Self retained internal ureteral stents: Use and complications: Mardis HK: AUA update series,
1997, Lesson 29, Volume XVI.
39. Ringel A, Richter S, Shalev M, Nissenkorn I. Late complications of ureteral stents. Eur Urol 2000; 38:41-
44.
40. Watson G. Problems with double-J stents and
nephrostomy tubes. J Endourol 1997; 11:413-417.
41. Hood CG, Dyer RB, Zagoria RJ. Complications of ureteral stenting. Appl Radiol 1990; 19:35-42.
42. Pollard SG, MacFarlane R. Symptoms arising from double-J ureteral stents.J Urol 1988; 139:37-38.
43. Bregg K, Riehle RA, Jr. Morbidity associated with indwelling internal ureteral stents after shock wave
lithotripsy. J Urol 1989; 141:510-512.
44. Mosli HA, Farsi HMA, Al-Zimaity F, Salem TR, Al-
Zamsami MM.Vesicoureteral reflux in patients with double pigtail stents. J Urol 1991;146:966-969.
45. Staton JW, Kropp KA. Proximal ureteral stent migration: an avoidable complication? J
Urol 1996; 155:58-61.
46. Somers WJ. Management of forgotten or retained
indwelling ureteral stents.Urology 1996; 47:431-435.
47. Chin JL, Denstedt JD. Retrieval of proximally
migrated ureteral stents. J Urol 1992; 148:1205- 1206.
48. Patel U, Kellett MJ. The misplaced double J ureteric stent: technique for repositioning using the nitinol
“gooseneck” snare. Clin Radiol 1994; 49:333-336.
49. Salazar JE, Johnson JB, Scott RL. Perforation of renal
pelvis by internal ureteral stents. AJR Am J Roentgenol 1984; 143:816-818.
50. Hepperlen TW, Mardis HK, Kammandel H. Self-
retained internal ureteral stents: a new approach. J Urol 1978; 119:731-734.
51. Schlick RW, Planz K. In vitro results with special
plastics for biodegradable endoureteral stents. J Endourol 1998; 12:451-455.
52. Mardis HK, Kroeger RM, Hepperlen TW, et
al. Polyethylene double-pigtail ureteral stents. Urol
Clin North Am 1982; 9:95-101.
53. El-Faqih SR, Shamsuddin AB, Chakrabarti A, et
al. Polyurethane internal ureteral stents in treatment of
stone patients: morbidity related to indwelling times. J Urol 1991; 146:1487-1491.
54. Gibbons RP. Gibbons ureteral stents. Urol Clin N Am 1982; 9:85-88.
55. Lennon GM, Thornhill JA, Sweeney PA, et
al. ‘Firm’ versus ‘soft’ double pigtail ureteric stents: a
randomized blind comparative trial. Eur
Urol 1995;28:1-5.
56. Joshi HB, Stainthrope A, Keeley FX, Jr, MacDonagh
R, Timoney AG.Indwelling ureteral stents: evaluation of quality of life to aid outcome analysis.J
Endourol 2001; 15:151-154.
57. Singh I, Gupta MP, Hemal AK, et al. Severely
encrusted polyurethane ureteral stents: management and analysis of potential risk
factors. Urology2001; 58:526-531.
International Journal of Scientific & Engineering Research, Volume 4, Issue 9, September-2013 2289
ISSN 2229-5518
58. Zisman A, Siegel YI, Siegmann A, Lindner A. Spontaneous ureteral stent fragmentation. J Urol 1995; 153:718-721.
59. Bergqvist D, Parsson H, Sherif A. Arterio-ureteral fistula: a systematic review. Eur J Vasc Endovasc Surg 2001; 22:191-196.
60. Kar A, Angwafo FF, Jhunjhunwala
JS. Ureteroarterial and ureterosigmoid fistula associated
with polyethylene indwelling ureteral stents. J Urol 1984;132:755-757.
61. Teuton ME, Viner MA, Zuckerman HL, Butler
DL. Ureteroiliac vein fistula associated with a
polyethylene indwelling ureteral stent. J Urol 1987; 137:975-976.
62. Furio Cauda, Valentina Cauda, Cristian Fiori, Barbara Onida, Edoardo Garrone, F; Cauda, V; Fiori, C; Onida, B; Garrone, E (2008), "Heparin Coating on Ureteral Double J Stents Prevents Encrustations: An in Vivo Case Study.", J Endourol. 22 (3): 465–
472, doi:10.1089/end.2007.0218, PMID 18307380.
63. Lingeman JE, Schulsinger DA, Kuo RL. Phase I
trial of a temporary ureteral drainage stent. J
Endourol 2003; 17:169.
64. Hadaschik BA, Paterson RF, Fazli L, et al.
Investigation of a novel degradable ureteral stent
in a porcine model. J Urol 2008; 180:1161.
65. Chew BH, Paterson RF, Clinkscales KW, et al. In
vivo evaluation of the third generation
biodegradable stent: a novel approach to avoiding
the forgotten stent syndrome. J Urol 2013; 189:719.
66. Hendlin K, Korman E, Monga M. New metallic
ureteral stents: improved tensile strength and
resistance to extrinsic compression. J Endourol
2012; 26:271.
67. Benson AD, Taylor ER, Schwartz BF. Metal ureteral stent for benign and malignant ureteral obstruction. J Urol 2011; 185:2217.
68. Goldsmith ZG, Wang AJ, Bañez LL, et al.
Outcomes of metallic stents for malignant ureteral
obstruction. J Urol 2012; 188:851.
69. Lang EK, Irwin RJ, Lopez-Martinez RA, et
al. Placement of metallic stents in ureters obstructed by carcinoma of the cervix to maintain renal function in
patients undergoing long-term chemotherapy. AJR Am
J Roentgenol 1998;171:1595-1599.
70. Modi AP, Ritch CR, Arend D, et al. Multicenter
experience with metallic ureteral stents for
malignant and chronic benign ureteral obstruction. J Endourol 2010; 24:1189.
71. Kulkarni R, Bellamy E. Nickel-titanium shape memory alloy Memokath 051 ureteral stent for managing long-term ureteral obstruction: 4-year
experience.J Urol 2001; 166:1750-1754.
72. Calleary JG. Chronic indwelling ureteral stents--
what is the optimal approach? J Urol 2011;
185:2016.
73. Chen HC, Shen SH, Wang JH, et al. Parallel second stent placement for refractory ureteral stent malfunction in malignant ureteral obstruction. J Vasc Interv Radiol 2011; 22:1012.
74. Riedl CR, Witkowski M, Plas E, Pflueger H.
Heparin coating reduces encrustation of ureteral
stents: a preliminary report. Int J Antimicrob
Agents 2002; 19:507.
75. Krambeck AE, Walsh RS, Denstedt JD, et al. A novel drug eluting ureteral stent: a prospective, randomized, multicenter clinical trial to evaluate the safety and effectiveness of a ketorolac loaded ureteral stent. J Urol 2010; 183:1037.
76. Tenke P, Riedl CR, Jones GL, et al. Bacterial biofilm
formation on urologic devices and heparin coating as preventive strategy. Int J Antimicrob Agents
2004; 23 Suppl 1:S67.
77. Giannarini G, Keeley FX Jr, Valent F, et al.
Predictors of morbidity in patients with indwelling
ureteric stents: results of a prospective study using the validated Ureteric Stent Symptoms Questionnaire. BJU Int 2011; 107:648.
78. Park SC, Jung SW, Lee JW, Rim JS. The effects of tolterodine extended release and alfuzosin for the
treatment of double-j stent-related symptoms. J Endourol 2009; 23:1913.
79. Lee SJ, Yoo C, Oh CY, et al. Stent Position Is More Important than α-Blockers or Anticholinergics for Stent-Related Lower Urinary Tract Symptoms after Ureteroscopic Ureterolithotomy: A Prospective
Randomized Study. Korean J Urol 2010; 51:636.
80. Norris RD, Sur RL, Springhart WP, et al. A
prospective, randomized, double-blinded placebo-
controlled comparison of extended release
oxybutynin versus phenazopyridine for the
management of postoperative ureteral stent discomfort. Urology 2008; 71:792.
81. Beddingfield R, Pedro RN, Hinck B, et al.
Alfuzosin to relieve ureteral stent discomfort: a
prospective, randomized, placebo controlled
study. J Urol 2009; 181:170.
82. Damiano R, Autorino R, De Sio M, et al. Effect of
tamsulosin in preventing ureteral stent-related
morbidity: a prospective study. J Endourol 2008;
22:651.
83. Wang CJ, Huang SW, Chang CH. Effects of tamsulosin on lower urinary tract symptoms due to double-J stent: a prospective study. Urol Int
2009; 83:66.
84. Franczyk J, Gray RR. Ureteral stenting in urosepsis: a cautionary note.Cardiovasc Intervent
Radiol 1989; 12:265-266.
85. Wolf, JS, Bennett, CJ, Dmochowski, RR et al. The
best practice policy statement of urologic surgery antimicrobial prophylaxis. American Urological Association, 2008. auanet.org/content/guidelines- and-quality-care/clinical-guidelines/main-
IJSER © 2013 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 4, Issue 9, September-2013
ISSN 2229-5518
2290
reports/ antimicroprop08.pdf (Accessed on
February 11, 2ffi0).
86. Kehinde EO, Rotimi VO, Al-Hunayan A, et al.
Bacteriology of urinary tract infection associated with indwelling J ureteral stents. J Endourol 2004; 18:891.
IJSER lb) 2013
http://www.ijserorq