International Journal of Scientific & Engineering Research, Volume 3, Issue 9, September-2012 1
ISSN 2229-5518
Pure Embryonal Carcinoma Testis With Inguinal
Lymph Node Metastasis- Rare Finding
Dr Ashima chugh, Dr Deepti Aggarwal, Dr Harsh Patel
—————————— ——————————
Embryonal carcinoma is a type of non-seminoma is present to some degree in about 40% of testicular tumors, but pure em- bryonal carcinomas occur only 3% to 4% of the time. Embryonal carcinoma tends to occur at a young age, the average age being
31 years. Metastasis of testicular cancer to inguinal lymph node rarely occurs, particularly in patients without any prior surgery
in inguinal and scrotal region. Based on histological types, non-seminoma cancer has higher incidence of inguinal metastasis (4.9%) compared to seminoma (0.5%). An embryonal carcinoma is an aggressive tumor due to its tendency to early hematogen- ous spread emphasizing the need for early detection and treatment. Fine needle aspiration is an excellent cytological method for the early diagnosis of embryonal carcinoma, based on which the patient can be spared the morbidity and expense of extensive surgical procedures.
IJSER © 2012
International Journal of Scientific & Engineering Research, Volume 3, Issue 9, September-2012 2
ISSN 2229-5518
A 22-year-old male presented at the surgery OPD of our hospital with left inguinal swelling.
Physical examination did not show inguinal hernia, CVA tenderness, varicocele. The inguinal swelling measured 3X4 cm, was
firm in consistency, fixed to the underlying tissue, and was non tender with prominence of overlying veins. The patient was subjected to FNAC.
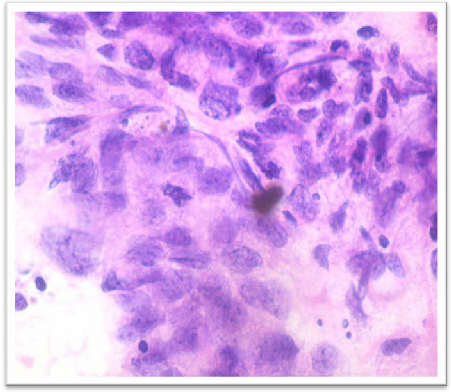
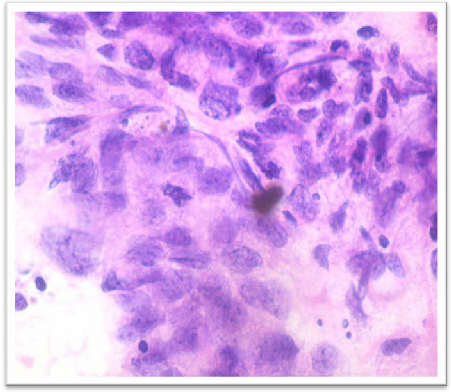
CYTOLOGY REPORT
The smears were cellular showing syncytial clusters of anaplastic tumor cells exhibiting moderate amount of pleomorphism and anisonucleosis.The primitive and pleomorphic-appearing epithelial cells dispersed singly were round to irregular with vesicular nuclei and prominent nucleoli. A diagnosis of a poorly differentiated neoplasm suggestive of embryonal carcinoma, was given. With these cytological findings, the patient was evaluated in detail and a mass was detected in the left testis.
Alfa fetoprotein & Beta – hcG levels were found to be raised.
USG report suggested malignancy. T2 weighted MRI showed low intensity masses suggesting malignant tumors. Biopsy of the testicular mass confirmed the cytological diagnosis of an embryonal carcinoma.
DISCUSSION
IJSER © 2012
International Journal of Scientific & Engineering Research, Volume 3, Issue 9, September-2012 3
ISSN 2229-5518
Testicular germ cell tumors are the most commonly occurring neoplasm in young males.1Lymphatic spread is common to all
testicular tumors; sequential spread, initially involving the retroperitoneal, para-aortic and subsequently the mediastinal and supraclavicular lymph nodes, is typical. Hematogenous spread is also possible, primarily to the lungs, but also to the liver, brain and skeleton. Metastasis of testicular cancer to inguinal lymph node rarely occurs, particularly in patients without any prior surgery in inguinal and scrotal region. Metastasis to inguinal lymph node may be caused by scrotum involvement or tunica va- ginalis by the primary tumor, previous inguinal or scrotal surgery or retrograde spreading of lymphatic system by accumulation of massive lymph node.2This patient had not had any treatment on his inguinal region before and the surgery was performed by trans-inguinal approach. Therefore, the metastasis may possibly result from the infiltrating spermatic cord, tunica vaginalis or retrograde spread of lymphatic system due to lymph node accumulation. Fine needle aspiration along with tumor markers
study is an excellent cytological method for the early diagnosis of embryonal carcinoma, based on which the patient can be
spared the morbidity and expense of extensive surgical procedures. It provides an option of early treatment and more life sav-
ing. The overwhelming majority of germ cell tumors are malignant and they are curable. 3 The high sensitivity of germ cell tu- mor to platinum based chemotherapy, together with radiation and surgical measures leads to high cure rate of ≥99% in the early stages, 90%, 75-80% and 50% in advanced disease with 'good' 'intermediate' and 'poor' prognostic criteria (International Germ Cell Cancer Consensus Group IGCCCG classification) respectively.1
CONCLUSION
Pure embryonal carcinomas are rare tumors metastasizing to inguinal lymph nodes. Early correct diagnosis by Fine Needle As- piration and tumor markers can save life of the patient. Fine needle aspiration is a quick and accurate tool for early diagnosis of metastasizing germ cell tumors. Chemotherapy with surgery and radiotherapy can be urgently started in such cases for saving life of the patient.
FIGURES
IJSER © 2012
International Journal of Scientific & Engineering Research, Volume 3, Issue 9, September-2012 4
ISSN 2229-5518
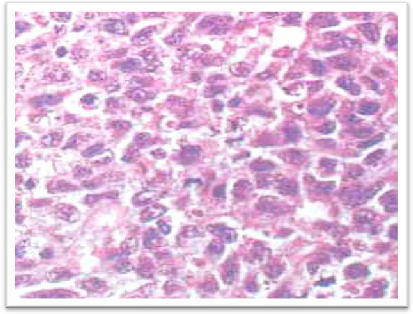
Figure1 - The smear from metastatic embryonal carcinoma shows fragment of large malignant cells with vesicular nuclei, coarse chromatin, prominent nucleoli; prominent cytoplasmic vacuolation( H & E 40x).
Figure 2- The section shows histomorphology of syncytial clusters of anaplastic primitive and pleomorphic-appearing epi- thelial cells tumor cells exhibiting moderate in microglandular pattern and dispersed singly . the cells are round to irregular with vesicular nuclei and prominent nucleoli suggesting poorly differentiated carcinoma most probably embryonal carci- noma (H&E 40x).
REFERENCES
IJSER © 2012
International Journal of Scientific & Engineering Research, Volume 3, Issue 9, September-2012 5
ISSN 2229-5518
1. Schmoll HJ, Souchon R, Krege S, Albers P, Beyer J, Kollmannsberger C, et al . European consensus on diagnosis and
treatment of germ cell cancer: A report of the European germ cell cancer consensus group (EGCCCG). Ann Oncol
2004;15:1377-99
2. Richie JP, Steele GS. Neoplasm of testis. In: Walsh PC, Retik AB, Vaughan ED Jr, et al, eds. Campbell’s urology. 8th ed.
Philadelpia: WB Saunders; 2002.
3. Yanardag H, Giinas Y. Diagnosis of a case of testicular embryonal carcinoma by bronchial biopsy. Int J Urol 2003;1:2.
IJSER © 2012